Clarissa A. Kussin, ND, FMCHC, ERYT-500
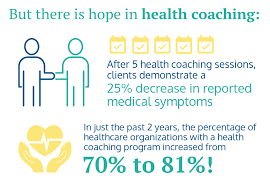
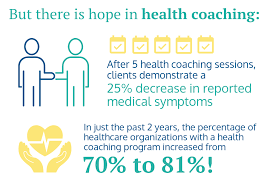
New Year’s is the time when everyone is looking toward the year ahead and all that they want to achieve. While people make resolutions with the best of intentions, few follow through and achieve their goals. This is where health coaching comes in handy.
Health coaches help support clients as they work toward making sustainable lifestyle changes. They are passionate about helping others live happier and healthier lives. This includes helping them stick to New Year’s resolutions. Whether you want to reduce stress, eat better, or move more, health coaches can guide the way.
The Power of Personalized Guidance:
A health coach is your dedicated partner on your wellness journey, offering personalized guidance that goes beyond generic advice. They work with you to create a tailored plan based on your unique needs, preferences, and health goals.
Medical Benefits of Having a Health Coach:
- Weight Management: Numerous studies have shown that individuals working with health coaches are more successful in achieving and maintaining a healthy weight. A health coach helps you develop sustainable habits, making weight management more than just a short-term goal.
- Chronic Disease Prevention and Management: Health coaches play a crucial role in preventing and managing chronic conditions such as diabetes, hypertension, and heart disease. Their guidance extends beyond conventional medical advice, focusing on lifestyle changes that can have a profound impact.
- Stress Reduction and Mental Well-being: Mental health is an integral part of overall well-being. Health coaches help you navigate stressors, offering support and strategies to enhance mental resilience. This holistic approach contributes to improved mental well-being.
- Improved Physical Fitness: A health coach can assist in developing personalized guidelines to follow that can help your fitness professional tailor your fitness routine to suit your lifestyle and preferences. Regular physical activity is linked to numerous health benefits, including improved cardiovascular health, increased energy levels, and better mood.
- Improved Sleep: Getting quality sleep is crucial for our physical and mental well-being. It affects our mood, concentration, and overall health. From creating a bedtime routine to sticking to a sleep schedule, there are many ways you can improve your quality of sleep. Health coaches may suggest options such as avoiding screens a few hours before bed. Perhaps practicing mindfulness in the evening will quiet a busy mind. Even something as simple as lowering the light in your room at night to trigger your sleep cycle are a small change that can result in a big outcome.
How to Get Started:
If you’re ready to experience the transformative benefits of health coaching, reach out to us today! Our team of experienced health coaches is here to guide you on your journey to optimal health. Call 919.999.0831 to get scheduled.
Remember, investing in your health is an investment in a brighter and more fulfilling future.
To your health and happiness!
References:
Wing, R. R., et al. (2018). Intensive lifestyle intervention in type 2 diabetes. New England Journal of Medicine.
Ockene, I. S., et al. (2007). The role of counseling in the promotion of healthy behaviors in adults. JAMA.
Huffman, J. C., et al. (2018). The role of stress and psychosocial interventions in cancer. Current Psychiatry Reports
Warburton, D. E. R., et al. (2006). Health benefits of physical activity: the evidence. Canadian Medical Association Journal
Your Partner In Health,
Clarissa A. Kussin, ND, FMCHC, ERYT-500